Hospital Transformation Program

The Hospital Transformation Program (HTP) is a value-based program administered by the Colorado Medicaid program for hospitals caring for Medicaid clients. HTP requests that hospitals in the state of Colorado focus on the following primary goals:
- They have experience taking care of many long-term conditions, including diabetes, high blood pressure, asthma, arthritis, and depression.
- If you need to see a specialist, your PCP will help you find the right one and talk with them about your care.
- Most PCPs see you in the clinic, but some will also see you in the hospital. They will ensure that you receive the proper care after a surgery, accident, or serious illness.
- Some PCPs have extra training in areas like women's health, addiction, nutrition, or skin care.
- They can often see you when you're sick. This saves a trip to the urgent care or emergency room. If they suspect that something more serious is happening, they can offer advice on where to go and the safest way to get there.
- PCPs ensure you receive the appropriate health exams, tests, and vaccines. For example, they let you know when it's time for a flu shot, cancer screening, blood test, or checkup.
- They are your partner in helping you to eat healthy foods, exercise, quit smoking, manage stress, and much more.
- They work with a team of staff to answer your questions, make appointments, and support your health.
For more detailed information, please visit this link: Colorado Hospital Transformation Program | Colorado Department of Health Care Policy & Financing.
Spanish Peaks Regional Health Center's mission, vision, and values align with the goals of the Hospital Transformation Program. Over the next five years (2021-2026), we will focus on building, implementing, and partnering with the community.
Program Areas Include:
Please click on the program areas to get more information
There is growing evidence that when a patient with a chronic disease, such as diabetes, heart failure, or COPD, sees their family doctor or within 30 days of their Emergency Department discharge, their risk of death or re-hospitalization is significantly reduced. Such patients are often safe to discharge after an ER assessment; however, prompt follow-up is always recommended, as they may require additional tests, a referral to a specialist, or ongoing management of their chronic illness to prevent worsening, even with good care in the Emergency Department.
Patients seen by their own doctors after an ER discharge are more likely to be taking the necessary medications and to have undergone needed diagnostic testing than those who miss follow-up care, suggesting that such patients have risk factors that can be improved through prompt follow-up.
Spanish Peaks Regional Health Center Plan:
We are hiring new medical providers for the Family Clinic, La Veta Clinic, and Specialty Clinic to serve the community.
Process: We are reworking clinic hours and provider availability to improve access to care and expand appointment availability, including same-day appointments.
Technology: We utilize our Electronic Health Record to identify patients who have been seen in the Emergency Department and prioritize their follow-up appointments as medically necessary.
Community Engagement: We will educate the community on the importance of this initiative and the importance of having a Primary Care Physician.
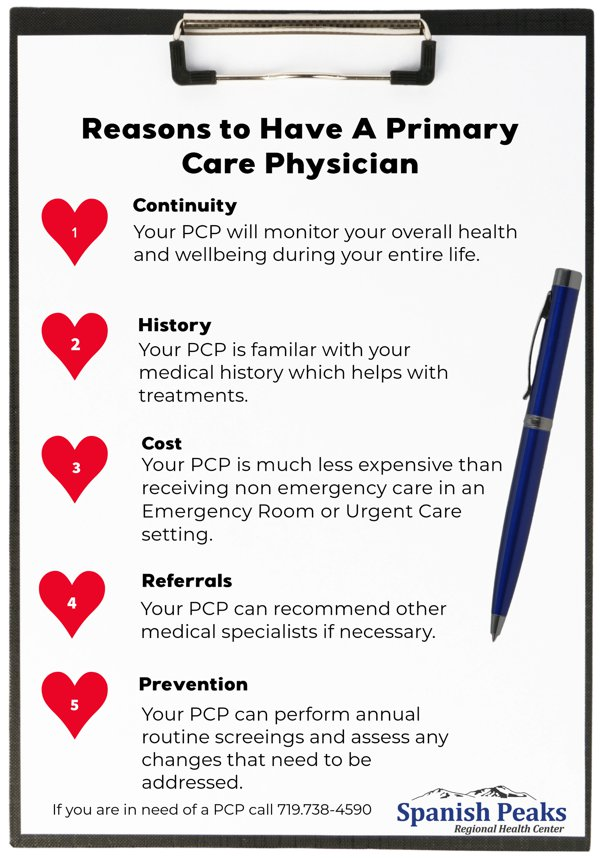
Offer: A Primary Care Physician (PCP) is a licensed healthcare professional who takes care of the whole person. Over time, they get to know all about you and your health. PCPs are trained to keep you well, but they also take care of you when you're sick.
Most PCPs are physicians. You may see the letters "MD" or "DO" after their names. However, Nurses with advanced training, such as advanced practice nurses (APNs), nurse practitioners (NPs), or certified nurse-midwives (CNMs), also provide primary care. A physician assistant (PA) may also be a PCP. These providers work directly with our physicians.
PCPs have a variety of jobs and roles:
- They have experience taking care of many long-term conditions, including diabetes, high blood pressure, asthma, arthritis, and depression.
- If you need to see a specialist, your PCP will help you find the right one and talk with them about your care.
- Most PCPs see you in the clinic, but some will also see you in the hospital. They will ensure that you receive the proper care after surgery, accident, or serious illness.
- Some PCPs have extra training in areas like women's health, addiction, nutrition, or skin care.
- They can often see you when you're sick. This saves a trip to the urgent care or emergency room. If a suspect feels that something more serious is happening, they can give you advice on where to go and the safest way to get there.
- PCPs ensure you receive the appropriate health exams, tests, and vaccines. For example, they let you know when it's time for a flu shot, cancer screening, blood test, or checkup.
- They are your partner in helping you to eat healthy foods, exercise, quit smoking, manage stress, and much more.
- They work with a team of staff to answer your questions, make appointments, and support your health.
Spanish Peaks Regional Health Center Plan:
We are hiring new medical providers for the Family Clinic, La Veta Clinic, and Specialty Clinic to care for our community.
Process: We are reworking clinic hours and provider availability to improve access to care and expand appointment availability, including same-day appointments.
Technology: We utilize our Electronic Health Record to identify patients who are due for an annual wellness visit and prioritize their appointments as medically necessary.
Community Engagement: We will educate the community on the importance of this initiative and the importance of having a Primary Care Physician. (Insert Poster here-PCP SPRHC)

Transitional Care Management (TCM) addresses the safe handoff of a patient from one setting of care to another. Most often, this handoff involves a patient moving from an acute, inpatient setting to an outpatient care environment, i.e., back to the care of their PCP. During transitions of care, primary care physicians (PCPs) often encounter care gaps that are beyond their control due to factors such as inaccessible patient records, unclear discharge care plans, or limited effort by others to engage the primary care team or the patient and their caregivers. Patients with chronic conditions, organ system failure, or frailty are at the most significant risk during this period, including readmission to the hospital. The sharing of medical information between different hospitals, providers, and medical services is referred to as "Interoperability."

Spanish Peaks Regional Health Center Plan:
People: We are training our teams to capture accurate information about you and your PCP when admitted so we know where to send your medical records.
Process: We are reaching out to PCPs outside our hospital to ensure we have the most accurate and up-to-date information for them.
Technology: We are using our Electronic Health Record to send a summary of care documents to your PCP upon your discharge from the hospital. We are also working to receive a summary of care documents from your PCP upon admission to the hospital.
Community Engagement: We will educate the community on the importance of having a Primary Care Physician and notify us of this information so that we can collaborate and communicate with your provider on your medical care.
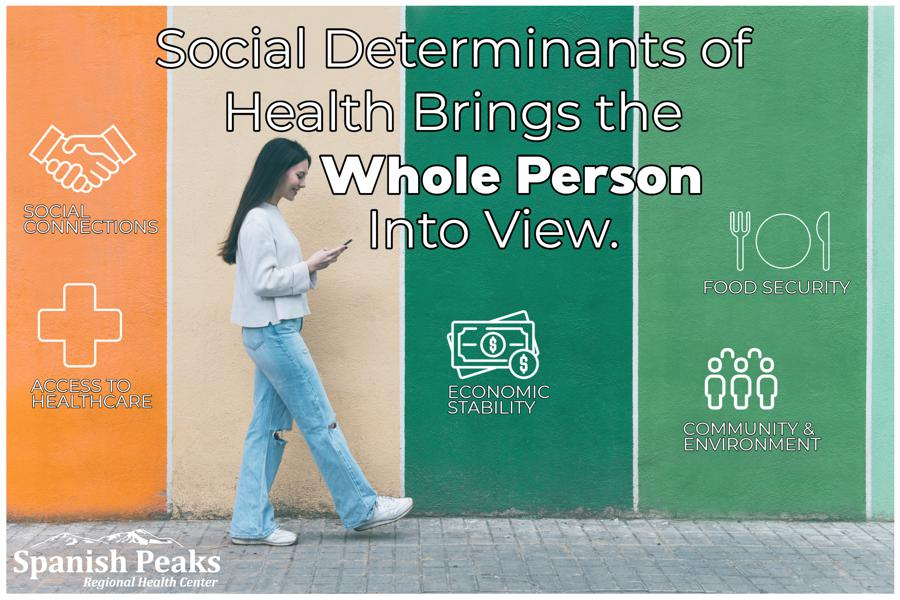
Having a clear understanding of our patients' socioeconomic needs is crucial to enhancing their health outcomes. Lack of food, housing, clean water, transportation, and employment, among other challenges, can have significant downstream effects on patients who are otherwise healthy. For those with chronic conditions, socioeconomic factors are even more crucial because they hinder lifestyle changes that are often first-line treatments for those conditions. For example, patients with type 2 diabetes may be unable to control their A1C if they cannot afford their medications or do not have access to healthy groceries.
Non-medical conditions that significantly impact health and quality of life are referred to as Social Determinants of Health (SDOH). According to the U.S. Department of Health and Human Services, SDOH falls into five categories: economic stability, healthcare access and quality, education access and quality, neighborhood and built environment, and social and community context. Within these categories are basic needs, including safety, transportation, food, and housing.
Spanish Peaks Regional Health Center Plan:
People: If you are admitted to Spanish Peaks Regional Health Center, our trained nurses may ask you specific questions about your needs in these social domains so that we can help match your needs to the appropriate community resources.
Process: For all patients, we will connect you with established community resources to support your recovery after discharge from the hospital. For Medicaid patients, we will also notify the Regional Access Entity (RAE), which coordinates your care and Medicaid benefits.
Technology: We utilize our Electronic Health Record to identify patients in need and coordinate their discharge plans.
Community Engagement: We will educate the community on the importance of this initiative and the importance of transparency and honesty in addressing their needs.
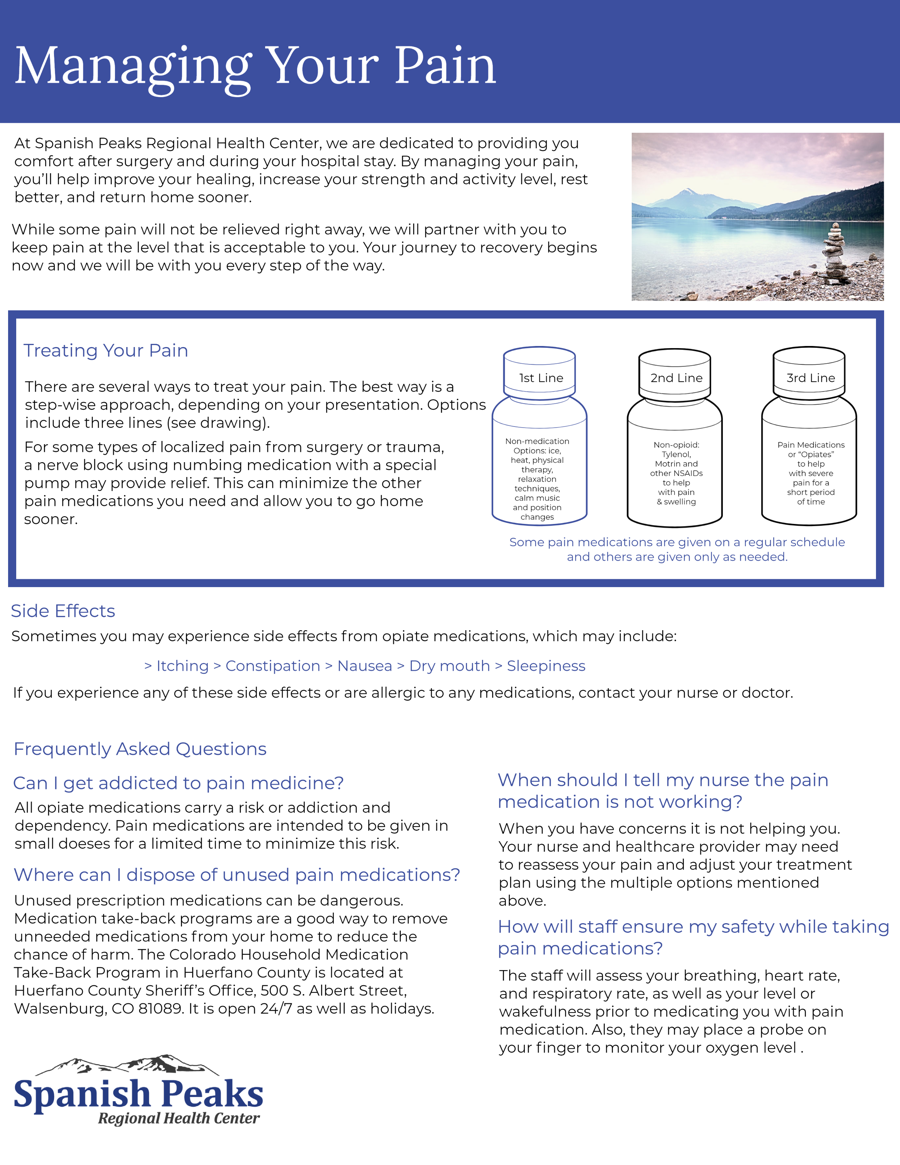
Opioids are a commonly prescribed class of medicine that is used for a short time to manage acute pain. Designed to target nerve cells and block pain signals, prescription opioids include codeine, morphine, oxycodone, and fentanyl. Prescription opioids may be used long-term in some instances, such as to treat pain related to advanced-stage cancer. The reason opioids typically are recommended as a short-term solution for acute - not chronic - pain is that they provide less relief over time.
Although opioid medicines can be effective, they come with risks and side effects, such as:
- Accidental overdose and death
- Constipation
- Depression
- Inability to urinate
- Excessive sleepiness
- Upset stomach
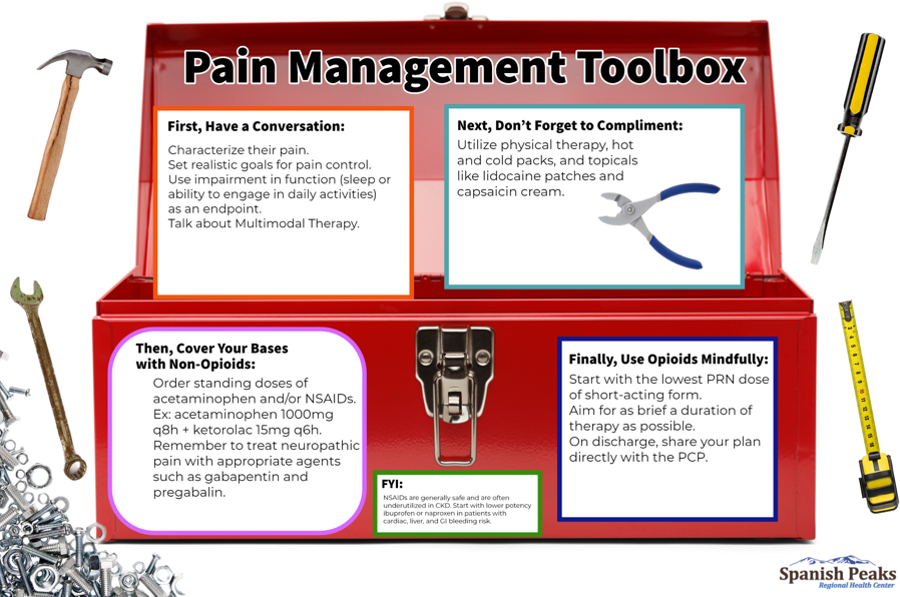
Opioids aren't the only option for pain treatment. Even if your health care provider has prescribed opioids to treat your pain, your care team has likely recommended that you also use nonopioid pain control. Having a holistic approach to treating pain not only reduces dependency on opioid medicines but also provides you with a variety of tools to address your pain.
- Acetaminophen, which you might know as Tylenol. There are many applications for this medication that can be used for acute and chronic pain.
- Antidepressants help regulate pain sensations in addition to mood. Antidepressants such as tricyclic antidepressants and serotonin and norepinephrine reuptake inhibitors can be used to treat chronic pain conditions such as fibromyalgia and migraines.
- COX-2 inhibitors inhibit a specific enzyme, which means reduced inflammation. COX-2 inhibitors are commonly used to treat chronic arthritis pain. An example is celecoxib.
- Gabapentinoids such as gabapentin and pregabalin reduce inappropriate nerve conduction found in conditions such as diabetic neuropathy and chemotherapy-induced nerve pain.
- Nonsteroidal anti-inflammatory drugs (NSAIDs), which you might know as aspirin, ibuprofen, or Ketorolac. Used for acute pain, NSAIDs help reduce fever, inflammation, and pain.
- Steroids are anti-inflammatory medicines that can help reduce acute pain after surgery or injury.
- Topical medicines are applied to the skin as an ointment, cream, or patch. Topical medicines such as lidocaine are used for muscle, joint, and skin pain.
Spanish Peaks Regional Health Center Plan:
People: We are training our ED providers and nurses on a multi-modal pain management strategy and a growing Alternatives to Opioids (ALTO) first medical practice.
Process: For all ED patients, we will do our very best to control your pain with non-opioid medications first to decrease your risk of side effects and addiction.
Technology: We are using our Electronic Health Record to identify vulnerable patients at risk of addiction or side effects, and minimize opioid use in those patients
Community Engagement: We will educate the community about the importance of this initiative and the risks associated with opioid use.
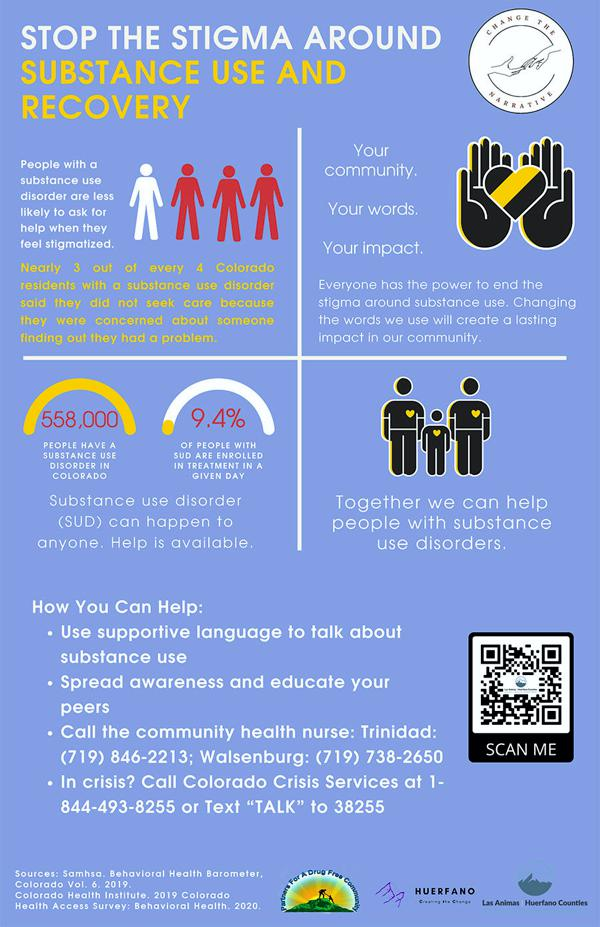
In 2016, 2.1 million people in the United States suffered from an opioid use disorder (OUD) related to prescription opioids, and 262,000 had an OUD related to heroin. One common treatment option for OUD is medication-assisted treatment (MAT), a treatment combining the use of medications (methadone, buprenorphine, or naltrexone) with counseling and behavioral therapies to sustain recovery.
The Spanish Peaks Regional Health Center Plan:
People: We are training our medical providers and nurses to identify patients struggling with Opioid Use Disorder and offer them Medication-assisted Treatment through our Family Clinic.
Process: For all MAT-eligible patients, we will connect you with local behavioral and counseling services through Crossroads and ongoing MAT therapy monitoring through the Front Range Clinic or Huerfano-Las Animal Health Department.
Technology: We are using our Electronic Health Record to identify vulnerable patients at risk of opioid addiction and minimize opioid use in those patients, as well as offer MAT therapy when medically appropriate.
Community Engagement: We will educate the community on the importance of this initiative and the serious risks of opioid use. We will work to decrease stigma and bias related to opioid addiction in the community.
Hospitals seeking to participate in the Hospital Transformation Program (HTP) are required to engage with community organizations and health neighborhoods as they plan for their participation in the HTP. The community engagement process is designed to build upon the strong spirit of collaboration within Colorado's Health System, as well as the efforts and partnerships already underway. Spanish Peaks will engage, consult, and be informed by health neighborhoods and community organizations to identify community needs and guide the transformation initiatives. We are committed to an inclusive and meaningful engagement.
Our current community advisors and key stakeholders include:
- Health Colorado, Health Solutions
- Front Range Clinic, Walsenburg
- Crossroads, Walsenburg
- Spanish Peaks Patient & Family Advocacy Council
- Huerfano County Communication Coalition / Chamber of Commerce
- Las Animas-Huerfano Health Department
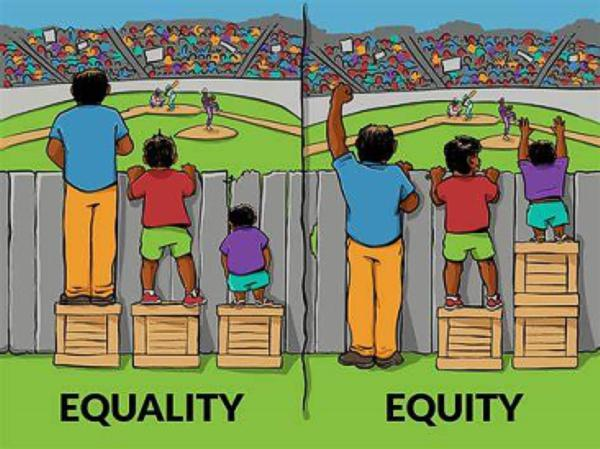
We engage with these groups quarterly, and once per year (Sept-Oct usually) host a Public Forum seeking direct community input into our program development. As our initiatives grow, we will assess our community impact through the lens of Equity and Diversity. Equity, diversity, and inclusion (EDI) is a conceptual framework that promotes the fair treatment and full participation of all people, especially those from populations that have historically been underrepresented or subject to discrimination due to their background, identity, disability, or other factors.
Equity involves providing resources according to need to help diverse populations achieve their optimal state of health and overall functioning.
Diversity refers to the representation or composition of various social identity groups in a workgroup, organization, or community.
Inclusion strives to create an environment that offers affirmation, celebration, and appreciation of diverse approaches, styles, perspectives, and experiences.
The Spanish Peaks Equity, Diversity, and Inclusion Community will analyze data to identify patients who may benefit from our initiatives and whom we have not been able to positively impact (yet).